Sometimes in healthcare, our need for immediate gratification causes more problems than solutions. We want something “fixed” instantly and want care available “immediately” regardless of the cost or effectiveness of the treatment.
We are a society of “now.”
Technology has advanced and fostered this “culture of instantaneousness.” However, what happens when these needs to have a “fix” come at a cost to others? What happens when the “fix” is only temporary?
There are many health conditions we could discuss where the easy fix is one that may not lead to long term change. You can bet that anything with lifestyle modification attached to it has another option that is easier than changing your health behaviors (e.g. a pill easier than weight loss).
We see this all the time in healthcare.
While losing weight, exercising and eating healthy may actually lead to the reversal of some health conditions, medications to control these conditions are often easier and help us have immediate change in our health. And this is often what we are demanding. When 40% of the time we die prematurely it is due to our behavior, it is time to examine the effectiveness of our interventions over their efficiency.
The problem is also seen in how we utilize the healthcare system. The emergency room is the epitome of instant gratification.
The Center for Disease Control has some excellent data on healthcare access and utilization. In one report, “Emergency Room Use Among Adults Aged 18–64: Early Release of Estimates From the National Health Interview Survey, January–June 2011, data show how translating our need for immediacy into healthcare is resulting in problems further down stream. Highlights from the report include:
About 79.7% of adults visited the emergency room due to lack of access to other providers, significantly more than the 66.0% who visited due to seriousness of the medical problem.
The most common reasons for the last emergency room visit were: only a hospital could help (54.5%), the doctor’s office was not open (48.0%), or there was no other place to go (46.3%).
Adults with unmet medical need were less likely than adults without unmet need to visit the emergency room because their doctor’s office was not open, and more likely to visit because they had no other place to go.
The graph to the right says it all. 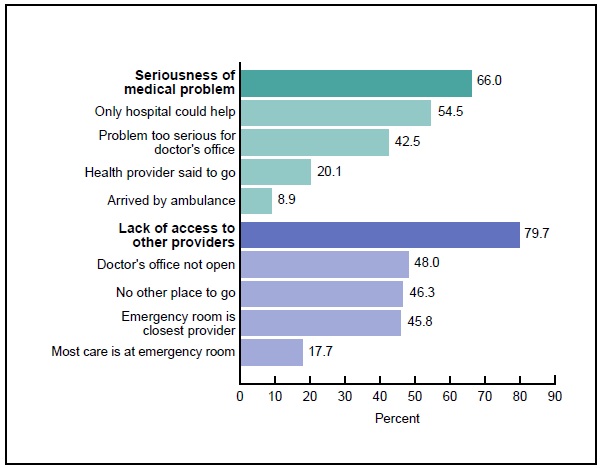
While many of the problems we face in healthcare do have to do with access, there are underlying issues here that drive our behavior in the healthcare system. Sometimes our beliefs about our health force us to that place where we want to have our needs addressed immediately. Part of the reason the emergency room is so appealing is that is will allow us to be seen by someone.
And so we go to the ER and wait.
And wait.
In some cases, this waiting can be hours on end. I am sure some of you see the irony in this (and have experienced this).
However, the emergency department has a function, and that function is to take care of emergencies. Unfortunately, as we have written about before and the graph shows, we go to the emergency room for the wrong reasons.
What can we do about this? How can we begin to address some of the underlying cultural reasons we want what we want and we want it now?
1) We can work within our communities to create a culture of health: Take for example 2040 Partners for Health. This Denver based organization has the mission to “advance the health and healthcare of area residents and employees by informing and facilitating health programs and policies, using Community-Based Participatory Research (CBPR), through a collaboration with the University of Colorado Anschutz Medical Campus, neighborhoods, and the Stapleton Foundation.” They work in the community to better understand what the community needs and then partners with others who can help study the problem, recommend solutions and make changes. If we want to talk about changing culture and creating one built around health (as opposed to sickness), we need to start local; we need to start in our own communities.
2) We can establish a relationship with a primary care provider: While many primary care providers may still need to refer patients to the emergency room, that is a different issue altogether than one where the patient simply goes to the emergency room to receive primary care services. The beauty of primary care is the relationship that is formed over time (we healthcare folks often call this continuity). Getting to know your primary care provider can be an important first step in changing how we address our own health. These providers can work with us over time on some of the more complicated changes we may need to make in our health.
3) We can become aware of our own healthcare story: Do you know your own healthcare footprint? Are you able to track where you have used services, when and how? These may seem like insignificant issues on the surface, but what happens when we start to recognize patterns in our own healthcare utilization (and behavior). Are we aware of how we use the system? Are we contributing to the culture of now in healthcare?
It is simply impossible for healthcare to be able to accommodate everyone all the time. There are not simply enough healthcare providers to go around (even if everyone had health insurance). It is also simply impossible for us to always expect that the easiest solution is the best one.
As we all work towards changing healthcare, let us not forget about the underlying culture of “now.”
OK, my instant coffee is ready – got to go.
